[There is a film] Why do I get diabetes without eating too much sweets?
Table of contents
"I don't like sweets at all, so why did I get diabetes?" This is a common and shocking question many people with type 2 diabetes ask upon diagnosis. This reflects a prevalent misconception: equating diabetes directly with "eating too much sugar." In fact, the causes of diabetes are far more complex than simply "eating sweets"; it's a disease caused by…Genetics, lifestyle, endocrine systemThis is the result of the long-term interaction of multiple factors. This article will delve into the reasons why people who don't eat sweets develop diabetes, and analyze the complete process from the incubation period to the onset of the disease through timelines and charts, finally providing clear prevention and management strategies.

Chapter 1: Debunking Myths—Diabetes is Not a Single Disease Caused by "Eating"
First, we must correctly understand the nature of "diabetes".
1. What is diabetes?
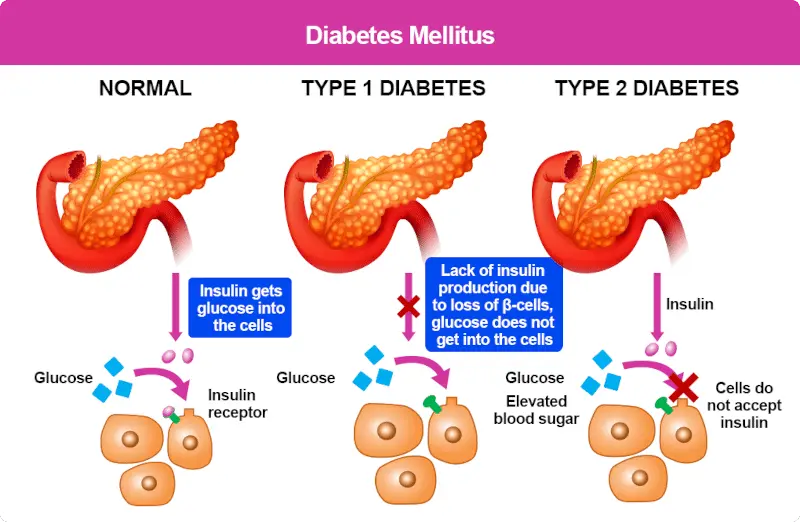
Diabetes is a chronic metabolic disease. The core problem is not "eating too much sugar," but rather the body's inability to effectively utilize or produce enough insulin. Insulin is a hormone secreted by the beta cells of the pancreas. It functions like a "key," unlocking cells and allowing glucose (blood sugar) from the blood to enter and be converted into energy. When this mechanism malfunctions, blood sugar accumulates in the blood, leading to hyperglycemia, which in turn causes long-term and severe damage to organs, blood vessels, and nerves throughout the body.
2. Types of Diabetes
- Type 1 diabetes: The autoimmune system mistakenly attacks and destroys the pancreas's beta cells, resulting in a near-complete inability to produce insulin. Patients must inject insulin for life. This type is less related to dietary habits and often develops at a young age.
- Type 2 diabetes: This accounts for over 90% of all diabetes cases (TP3T). The body develops "insulin resistance" (cells become insensitive to insulin, like a key not opening a lock), which may later be accompanied by insufficient insulin secretion. This is the type of diabetes most people who "don't eat sweets but still get diabetes," and its causes are extremely complex.
- Gestational diabetes: Temporary diabetes that occurs during pregnancy due to hormonal changes carries a higher risk of developing type 2 diabetes later in life.
- Other specific causal types: Caused by gene mutations, pancreatic diseases, drugs, etc.
The core of this article will revolve around...Type 2 diabetes.
Symptoms of acute complications of diabetes
| Symptoms | Performance |
|---|---|
| Diabetic ketoacidosis | The initial symptoms of "polyuria, polydipsia, polyphagia, and weight loss" worsen, followed by fatigue, drowsiness, headache, nausea, vomiting, rapid and deep breathing with a rotten apple odor on the breath, and later, severe dehydration, lethargy, and even coma. |
| Hyperosmolar hyperglycemia | Initially, patients present with polyuria, polydipsia, and loss of appetite, gradually developing severe dehydration and neuropsychiatric symptoms. They may become lethargic, irritable, or apathetic, or drowsy, eventually falling into a coma. In later stages, oliguria or even urinary retention may occur. |
Typical symptoms of diabetes
| Symptoms | Performance |
|---|---|
| polyuria | Increased frequency of urination, significantly increased urine volume, and some people may experience foamy or sweet-smelling urine. |
| Drink more | Frequent thirst, significantly increased water intake, and the thirst is not relieved even after drinking water. |
| Eat more | I often feel hungry and eat more than usual, but I still feel hungry again soon after eating. |
| Weight loss | Unexplained weight loss in a short period of time, even with normal or increased food intake, may still result in weight loss. |
| itchy skin | Dry, itchy skin, especially on the extremities or perineum, is a common symptom. Female patients may also experience vulvar itching due to irritation from urinary glucose, and may be complicated by Candida albicans infection. |
| Blurred vision | When blood sugar rises rapidly, it can alter the osmotic pressure of the aqueous humor and lens, causing refractive changes and resulting in blurred vision. |
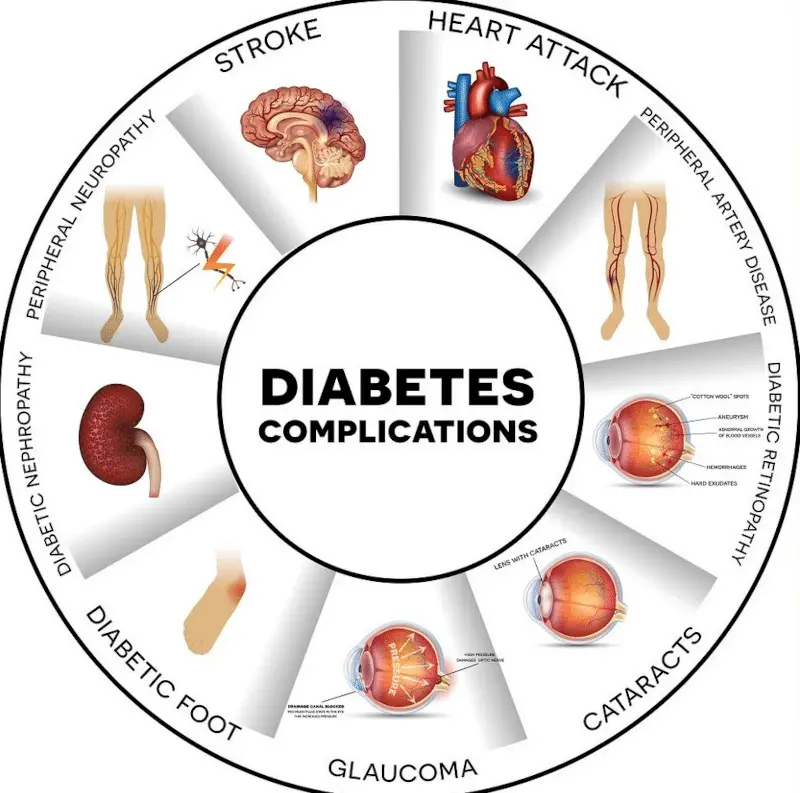
Symptoms of chronic complications of diabetes
| Symptoms | Performance |
|---|---|
| Diabetic nephropathy | In the middle and late stages, symptoms such as foamy urine, high blood pressure, and edema may appear, eventually leading to kidney failure. |
| Diabetic retinopathy | As the disease progresses, vision deteriorates to varying degrees, and objects appear distorted; in severe cases, blindness may occur. |
| Diabetic neuropathy | Peripheral neuropathy manifests as sensory abnormalities in the distal extremities, such as numbness, tingling, and decreased sensation; autonomic neuropathy can present with symptoms such as delayed gastric emptying, diarrhea, constipation, orthostatic hypotension, and urinary incontinence. |
| diabetic foot | Mild cases present with foot deformities, dry and cold skin, and calluses; severe cases may develop foot ulcers and gangrene. |

Chapter Two: Six Key Reasons Why People Develop Diabetes Even If They Don't Eat Sweets
Even without intentionally consuming sweets, the following factors can still silently push you towards the risk of diabetes.
1. The Trap of Refined Carbohydrates (Sugars)
This is the most crucial and most easily misunderstood point.Not eating sweets does not mean that your sugar intake is not excessive..
- What is refined sugar? This refers to processed carbohydrates with bran and fiber removed, which are rapidly broken down into glucose by the body, causing blood sugar levels to spike like a rollercoaster. For example:
- White rice, white noodles, white toast, white steamed buns
- Flour products: Bread, biscuits, cakes (even savory soda crackers), pizza
- Processed snacks: Potato chips and rice crackers (they taste salty, but the main ingredient is refined starch).
- Sugary drinks: Hand-shaken cups (even when ordered "less sugar" or "no sugar," the toppings such as tapioca pearls, taro balls, and red beans are already high in sugar), sports drinks, and packaged fruit juices.
- Why is it dangerous? Consuming large amounts of these high glycemic index (GI) foods over a long period forces pancreatic beta cells to work overtime, secreting large amounts of insulin to cope with soaring blood sugar. Over years or even decades, the cells gradually become "fatigued" and "numb" to high concentrations of insulin, resulting in "insulin resistance," a typical characteristic of prediabetes.
2. Hidden sugars are everywhere.
Many foods that taste "not sweet" or "salty" actually have a lot of added sugar to balance the flavor and enhance the texture.
- Sauces: Ketchup, barbecue sauce, salad dressing, pasta sauce
- Soup and dishes: Thick soup noodles, risotto sauce, sweet and sour dishes, braised pork
- Processed meat products: Sausage, ham, and meat floss
- Health food traps: Some yogurt, cereals, and energy bars
You may not be eating sugar directly, but these "hidden sugars" can cause you to ingest excessive amounts of sugar without realizing it.
3. The double-edged sword of fat: visceral fat is the real culprit.
- Obesity and Insulin Resistance: In particular, visceral fat, which accumulates in the abdomen, liver, and around the pancreas, is highly active and continuously releases free fatty acids and inflammatory substances (such as tumor necrosis factor-alpha). These substances interfere with insulin signaling within cells, exacerbating insulin resistance.
- Non-obese diabetes: It's worth noting that even with a normal weight (BMI standard), a high body fat percentage and insufficient muscle mass ("puffy body type") still pose a significant risk of disease. This is because muscle is the primary site for glucose metabolism, and low muscle mass means reduced glucose utilization.
4. Sedentary lifestyle and insufficient muscle mass
The sedentary lifestyle and lack of exercise among modern people are a major reason for the surge in diabetes cases.
- The importance of exercise: During exercise, muscle contraction activates a channel that does not rely on insulin (GLUT4 channel), which directly draws glucose from the blood for use, effectively lowering blood sugar.
- Muscles are a reservoir for blood sugar: The more muscle mass you have, the more glucose you can store and consume, the lower your insulin requirements, and the more stable your body's ability to regulate blood sugar. Lack of exercise leads to muscle loss and decreased function, exacerbating abnormal blood sugar metabolism.
5. Genetics and Family History
Type 2 diabetes has a strong genetic predisposition. If your parents or siblings have diabetes, your risk of developing the disease is several times higher than the general population. Genetics determines your "susceptibility" to insulin resistance, but this is not fate.Genetic factors are like a loaded bullet, while unhealthy lifestyle habits are the hand that pulls the trigger.
6. Stress and lack of sleep
- pressure: When under prolonged stress, the body secretes stress hormones such as cortisol and adrenaline. These hormones prompt the liver to break down stored glycogen into glucose and release it into the bloodstream to increase the body's energy to cope with crises, thus causing blood sugar levels to rise.
- Sleep: Insufficient sleep or poor sleep quality (such as sleep apnea) can affect the endocrine system, leading to increased cortisol and exacerbated insulin resistance. It can also disrupt the appetite-controlling hormones leptin and ghrelin, making people crave high-calorie, high-sugar foods.
Chapter 3: The Timeline of Diabetes Development—A Long Journey from Normal to Diagnosed
The onset of diabetes is not sudden, but a gradual process that lasts 10 to 15 years or even longer. The following diagram illustrates its typical developmental stages:
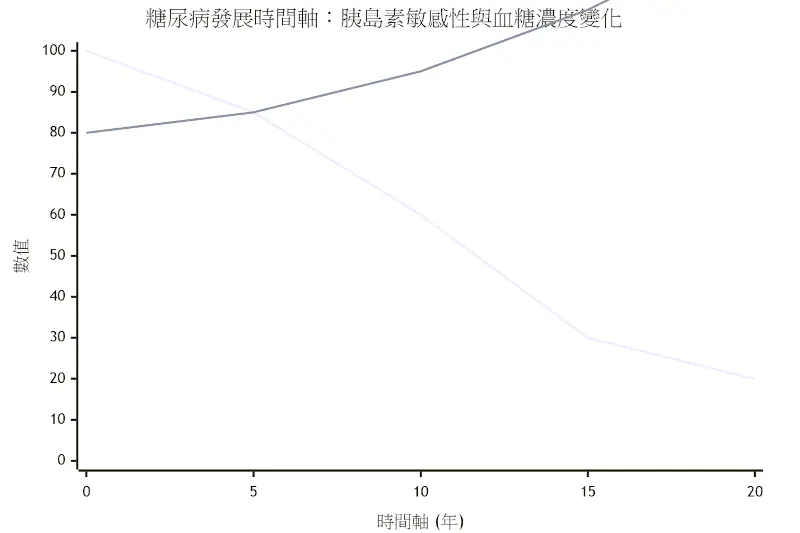
(This is for illustrative purposes only; actual values may vary from person to person.)
Phase 1: Insulin Compensation Period (Normal Blood Glucose)
- Physical changes: Insulin resistance begins to appear, and the cells' sensitivity to insulin gradually decreases (blue line in the above figure).
- The body's reaction: The pancreatic beta cells detect a trend of rising blood sugar, and then...CompensatoryThe body secretes more insulin in an attempt to forcefully maintain blood sugar within the normal range.
- Clinical manifestations: at this timeBlood sugar test completely normalHowever, the insulin concentration in the blood is already high. The patient is unaware of it, but diabetes has already been quietly developing.
Phase Two: Prediabetes
- Physical changes: As insulin resistance continues to worsen, pancreatic β cells begin to become fatigued and damaged after years of overwork, and their ability to secrete insulin gradually declines (the blue line declines rapidly).
- The body's reaction: Insulin secretion is insufficient to suppress postprandial blood sugar, and blood sugar begins to exceed the normal range, but has not yet reached the diagnostic criteria for diabetes.
- Impaired fasting glucose (IFG): Fasting blood glucose level between 100-125 mg/dL
- Impaired glucose tolerance (IGT): Two hours after the oral glucose tolerance test, blood glucose levels ranged from 140 to 199 mg/dL.
- Clinical manifestations: It is still possible to have no symptoms at all. This isThe final golden period for a turnaroundWith intervention in lifestyle habits, there is a high chance of recovery to normal.
Stage 3: Onset of Type 2 Diabetes
- Physical changes: Severe insulin resistance, coupled with significant decline in pancreatic β-cell function, resulting in insufficient insulin secretion (blue and orange lines intersect).
- The body's reaction: The body loses its ability to maintain stable blood sugar levels, resulting in persistently elevated blood sugar levels.
- Diagnostic criteria: Fasting blood glucose ≥ 126 mg/dL, or blood glucose ≥ 200 mg/dL 2 hours after oral glucose tolerance test, or glycated hemoglobin (HbA1c) ≥ 6.5%.
- Clinical manifestations: The typical symptoms of "three highs and one low" may begin to appear: increased appetite, increased thirst, increased urination, and weight loss, as well as fatigue and blurred vision. At this stage, although the disease can be controlled, it is difficult to "reverse".
Diabetic foot symptoms picturesDiabetic foot is one of the common and serious complications of diabetes. Mild cases may present with foot deformities, dry and cold skin, calluses, etc., while severe cases may develop foot ulcers and gangrene.

Images of diabetic retinopathyDiabetes can lead to a variety of eye diseases, such as retinopathy, which can cause cotton wool exudates, hemorrhages, microaneurysms, and abnormal blood vessel growth.


Chapter 4: How to Diagnose and Assess Risk? — Understanding Key Indicators
In addition to blood glucose levels, the following indicators are crucial for assessing diabetes risk:
1. Glycated hemoglobin (HbA1c)
Reflecting the pastTwo to three monthsAverage blood glucose concentration is the gold standard for assessing long-term blood glucose control.
- normal: < 5.7%
- Prediabetes: 5.7% ~ 6.4%
- diabetes: ≥ 6.5%
2. Insulin Resistance Index (HOMA-IR)
Calculated from fasting blood glucose and fasting insulin values, it can be used to assess the degree of early insulin resistance (the higher the value, the more severe the resistance).
3. Waist circumference and body fat percentage
Body mass index (BMI) is a better indicator of visceral fat accumulation than body weight.
- Men with a waist circumference ≥ 90 cm (approximately 35.5 inches)
- Women with a waist circumference ≥ 80 cm (approximately 31.5 inches)
Exceeding the above standards indicates excessive visceral fat, which greatly increases the risk.
To more clearly illustrate the data changes at each stage, please see the table below:
| stage | Fasting blood glucose (mg/dL) | Postprandial blood glucose (mg/dL) 2 hours after meal | Glycated hemoglobin (%) | Fasting insulin levels | Description of physical condition |
|---|---|---|---|---|---|
| normal | < 100 | < 140 | < 5.7 | normal | Insulin sensitive, blood sugar stable |
| Prediabetes | 100-125 | 140-199 | 5.7-6.4 | High | Insulin resistance occurs, and the pancreas compensates by secreting more insulin. |
| diabetes | ≥ 126 | ≥ 200 | ≥ 6.5 | High first, then low | Pancreatic failure, unable to secrete enough insulin |
Chapter 5: Prevention and Management Strategies – It's Never Too Late to Take Action
No matter what stage you are in, taking action will bring positive benefits.
1. Dietary adjustments: Emphasizing both quality and quantity
- Choose high-quality sugars: Replace refined starch withWhole grains(Brown rice, quinoa, oats, whole wheat bread)Legumes,tubersThese foods are rich in fiber and have a slow glycemic index.
- Smart order: try"Vegetables → Meat → RiceThe order of eating should follow this principle: starting with dietary fiber can slow down the absorption of subsequent sugars.
- Quit sugary drinks: This is the only and most effective step: Drink plenty of plain water, unsweetened tea, or black coffee.
- Learn to read nutrition labels: Pay attention to the content of "carbohydrates" and "sugars", rather than judging solely by taste.
2. Regular exercise: aerobic exercise combined with strength training.
- Aerobic exercise: At least 150 minutes of moderate-intensity exercise per week (such as brisk walking, swimming, or cycling) can effectively improve insulin sensitivity.
- Strength training: Increase muscle mass at least twice a week (such as weight training, resistance bands, squats, push-ups) to build more "glucose stores" for your body.
3. Control weight and reduce visceral fat
Weight loss (especially a reduction of 51%-71% of total body weight) can significantly improve insulin resistance. The goal is to maintain a BMI between 18.5 and 24 and keep waist circumference within the standard range.
4. Sufficient sleep and stress management
- Ensure 7-9 hours of quality sleep every night.
- Find stress-relief methods that suit you, such as meditation, yoga, deep breathing, or cultivating hobbies.
5. Regular health checkups
High-risk groups, especially those with a family history of the disease, should start having their fasting blood glucose and glycated hemoglobin checked annually from a young age to detect abnormalities and receive intervention as early as possible.

in conclusion
It's not uncommon or impossible for someone to develop diabetes without eating sweets. This profoundly illustrates that diabetes is a complex "lifestyle disease," its root cause being...Long-term insulin resistanceThe culprit isn't just the sugar in the sugar jar, but also the ubiquitous substances in our daily lives.Refined sugars, hidden sugars, excessive visceral fat, a sedentary lifestyle, and genetic predisposition.The combined effect of.
This disease develops slowly and insidiously, often lurking for years in the asymptomatic "prediabetes" stage. Instead of obsessing over the simple question of "whether or not to eat sweets," it's better to comprehensively examine your diet's texture, exercise habits, body shape, and stress levels. Understanding the complex mechanisms behind it and dispelling myths are the true keys to successfully preventing and effectively managing diabetes. Start taking action now to make positive changes for your health.
Further reading:



![[有片]把與生俱來的「好色」,用以點燃事業的雄心](https://findgirl.org/storage/2025/11/有片把與生俱來的「好色」,用以點燃事業的雄心-300x225.webp)


-300x225.webp)